
31 May To Your Health: Silent Killer, NASH!
Part-time Telluride local, Dr. Alan Safdi, is a world-renowned internist and gastroenterologist with encyclopedic knowledge of mind-body wellness and preventative medicine. He posts regularly on Telluride Inside… and Out under the banner of “To Your Health.” Dr. Alan’s blogs feature the most current information in his fields: health, wellness and longevity.
Links to Dr. Alan’s other podcasts and narratives on COVID-19 and more are here.
This week, Dr. Alan talks about one of the most dangerous consequences of being overweight or non-alcoholic steatohepatitis (NASH or NAFLD). The podcast is here.
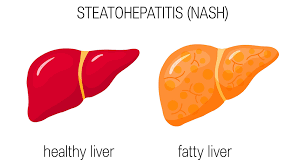
One of the especially dangerous health risks that results from being extremely overweight occurs when an obese individual begins to accumulate fat in their liver. This disease is commonly overlooked and can also occur in other settings such as lipid abnormalities, type 2 diabetes, polycystic ovarian disease, metabolic syndrome, and more.
This condition — non-alcoholic fatty liver disease or NAFLD—is the world’s most common chronic liver maladies and the primary underlying cause for liver transplants in children and adults.
Without such transplants, available to only a small percentage of patients, NAFLD over time can be fatal.In fact, (excluding alcohol-related liver damage) more than 30,000 people a year die from NAFLD.
NAFLD is rarely referred to the appropriate specialists or screened. Once the fatty liver with significant scarring occurs (fibrosis) it can relatively quickly progress to cirrhosis.
For years, the primary treatment for NAFLD has been through the use of various weight control methods: diet programs, exercise regimens, medications of limited benefit, bariatric surgery, and more. But once an individual develops progressive NAFLD, simply losing weight is not enough.
We need to focus on how excess caloric intake, particularly sugars or glucose, results in increased weight. That being overweight or obese with diabetes further pre-disposes a person to develop a fatty liver that can progress to inflammation, fibrosis and in a more severe cases cirrhosis.
Prevention as with cardiovascular diseases and diabetes is best achieved with lifestyle moderation; eating a healthy diet; exercising routinely; avoiding simple sugars; and maintaining a healthy target weight. When I think about nonalcoholic steatohepatitis (NASH), I think of a liver that is overtaxed from the delivery of too much metabolic substrate, that is, fat and carbohydrates.
Adipose Tissue
Adipose tissue plays an important role in NASH. Adipose tissue is a great place to store extra energy in the form of triglycerides. However, adipose tissue has limited storage capacity and, when that limit is reached, the tissue becomes stressed and begins to leak out fatty acids. It’s the liver that has to deal with those excess fatty acids in the blood.
Obesity and the 10%
Many patients with NASH also suffer from obesity. The data are clear that patients who lose 10% of their body weight experience enormous benefit for the liver. This is true even if, after that weight loss, the patient is still obese.
How do we explain that threshold, where the obesity can remain but the liver can benefit? In my assessment, it comes back to the adipose tissue’s capacity to store excess energy as triglycerides. That 10% weight loss helps because it can relieve stress on the adipose tissue such that it is no longer delivering excess fatty acids to the liver — the excess fats that ultimately cause NASH.
Although remaining obese has other problems, including physical impairments with back and knee injuries and the cultural disdain for obesity that our patients suffer with enormously, to me it is encouraging and fascinating that a 10% weight loss can have such profound physiologic benefits for the liver and likely other tissues. It’s as though it brings them back into that range where their adipose tissue is now healthier and not adversely affecting the liver.
One perspective is that diabetes is actually a disease of lipid metabolism, which promotes dysregulation of blood glucose levels. That is potentially highly relevant to treatment, as diabetes management has been very focused on glycemic control. However, if we do not control glucose the right way, then lipid storage becomes a bigger issue that leads to increased cardiovascular risk. As cardiovascular disease is a major cause of mortality in patients with diabetes and especially in patients with NASH, we do not want to exacerbate cardiovascular risk.
I emphasize the importance of limiting sugar intake, since the fructose in our table sugar and sweetened foods and beverages appears to play a major role in de novo lipogenesis, where the liver turns that sugar into fat.
Patients often do not realize how much sugar is in beverages such as sugar-sweetened tea or sodas. I explain that unless they are running marathons, their body does not need that sugar for energy, so the liver will have to deal with it by turning it into fat.
I also encourage my patients to lose weight in a gentle, kind way, acknowledging that for many achieving a 10% weight loss is an enormous challenge. I try to work with my patients and say, “Do the best you can; focus on healthy eating and try to be more active, whatever that means for you and whatever works for you.” Give the patients obtainable goals. Twenty-two minutes of exercise a day has tremendous benefits. Go over food logs and look for healthier substitutions and do this on a regular basis. Trying a Mediterranean Diet may be the easiest and healthiest diet to follow.
Weight loss is recommended for patients with non-alcoholic steatohepatitis (NASH), but the impact of weight change on disease activity remains unclear. We examined the association between weight change (gain/loss) and changes in biochemical and histological features of NASH. A recent study offers observational evidence, but strong observational evidence, that modest weight loss improves fibrosis and NASH. Combined with our previous meta-analysis of weight loss intervention trials, the evidence is now clear.This disease is a silent killer and is way too often overlooked. NASH does not manifest overtly early on and so we need better screening and referral when appropriate.
Dr. Alan Safdi:

Dr. Alan Safdi is board-certified in Internal Medicine and in Gastroenterology and is a Fellow of the American College of Gastroenterology. A proven leader in the healthcare arena, he has been featured on the national program, “Medical Crossfire” and authored or co-authored numerous medical articles and abstracts.
Safdi, a long-time Telluride local, has been involved in grant-based and clinical research for four decades. He is passionate about disease prevention and wellness, not just fixing what has gone wrong.
Dr. Alan is an international lecturer on the subjects of wellness, nutrition and gastroenterology.


Sorry, the comment form is closed at this time.